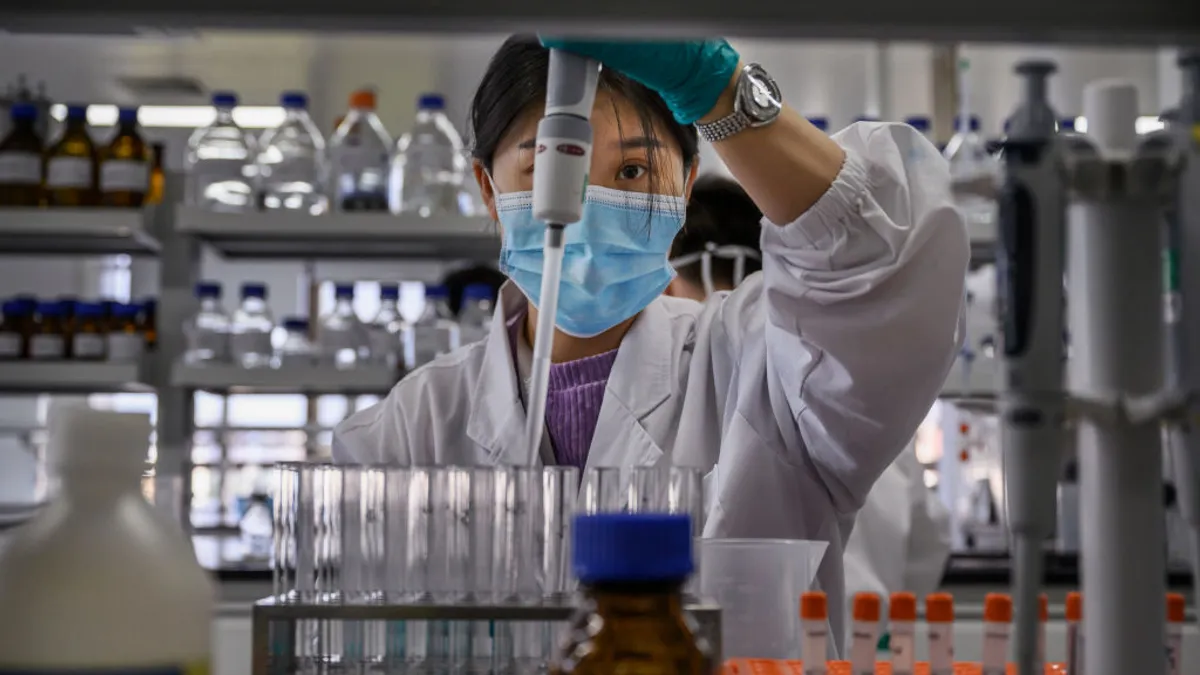
Like many drug discoveries throughout history, one of the medications still used today to treat schizophrenia came about accidentally.
In 1951, a scientist at a French pharmaceutical company created chlorpromazine, a drug he hoped would boost the effects of general anesthesia. What he produced was a calming, non-sedating treatment that drew the eye of a French army surgeon, Henri Laborit, who saw its potential for treating psychiatric conditions.
Thanks to this accidental discovery, chlorpromazine became the first in a new class of antipsychotic treatments for schizophrenia, a debilitating brain disorder marked by hallucinations, delusions, cognitive problems and functional challenges that affects about 24 million people worldwide.
While chlorpromazine marked a step forward for the field, scientific and clinical trial-related challenges such as slow recruitment and high drop-out rates have limited progress over the last 72 years. All of the current treatments for schizophrenia still act on the same dopamine D2 receptor as that first medication, said Andrew Miller, founder and president of research and development at Karuna Therapeutics. The pharmacology of chlorpromazine differs slightly from more recently approved schizophrenia treatments — some of them also modulate serotonin — but they all stick to the same basic playbook.
“Although the current range of antipsychotics may provide some relief from positive symptoms in schizophrenia patients, there are still several large unmet needs that remain,” said Summer Colling, an analyst at Citeline. “Some of the greatest unmet needs include drugs targeting the negative and cognitive symptoms of schizophrenia, drugs with improved tolerability, therapies encouraging enhanced compliance rates and more effective treatment options for refractory schizophrenia.”
However, the treatment landscape may change this year if Karuna’s drug KarXT gets the green light from the FDA, a decision expected in September. The drug, a muscarinic agonist, would be a first-in-class approval for schizophrenia.
Muscarinic receptors have become a tantalizing target for central nervous system disorders. But harnessing their potential power has been challenging. Muscarinic receptors aren’t only found in the brain, but exist in other places in the body, raising the potential for side effects. Karuna’s approach confines the drug’s effects to the brain.
The drug’s potential caught the eye of pharma giant Bristol Myers Squibb, which announced a $14 billion deal to acquire Karuna in December. The deal will give KarXT a leg up in the commercial arena considering BMS’s prior experience in multiple neuropsychiatric indications, Colling said.
KarXT has the potential to reduce positive, negative and cognitive symptoms of schizophrenia and also brings fewer problematic side effects, such as weight gain, metabolic side effects and uncontrolled movements, which often cause patients to stop taking them.
“What we see in our clinical trials is an absence of those side effects because we don't have that dopamine and serotonin-based pharmacology at the core of what KarXT is now,” Miller said. “That's not to say that KarXT is a side-effect-free treatment. We do generally have mild to moderate transient GI side effects.”
Companies close in on potential breakthroughs
While KarXT may be generating the most buzz, it’s not the only drug finding its way to the schizophrenia market, which could reach $7.11 billion by 2028. Much of the ongoing work is focused on shifting toward precision psychiatry, understanding the neurobiology of the condition instead of using symptoms to give patients better, more targeted treatments, Colling said.
“A lack of validated biomarkers is hindering the transition towards precision psychiatry,” Colling said. “There is also generally less investment in chronic conditions with large populations as firms need a broad commercial strategy and must be prepared to engage with many healthcare providers.”
Including KarXT, the pipeline comprises three drugs in the NDA stage, 12 in phase 3, seven in phase 2 and 15 in phase 1, according to Colling. Pipeline compounds are most commonly directed at legacy targets like dopamine and serotonin, she said. But others seek out novel schizophrenia targets, including muscarinic receptors, like KarXT, as well as the NMDA brain receptor, and D-amino-acid oxidase, which blocks an enzyme that can interfere with brain function.
“The closest competitors to KarXT are Cerevel Therapeutics’ emracladine and Neurocrine’s NBI-1117568, which are both in phase 2 development behind KarXT in the race for FDA approval,” Colling said. “Emraclidine, which also targets the muscarinic receptor, is particularly promising as it is differentiated from KarXT by its dosing frequency (once daily versus twice daily), its lack of titration needs and, potentially, its stronger gastrointestinal side-effect profile.”
AbbVie plans to acquire emracladine as part of an $8.7 billion acquisition of Cerevel. But the deal may be delayed after an increasingly aggressive Federal Trade Commission requested additional information.
Another promising contender is Acadia’s Nuplazid, which targets negative symptoms, such as emotional withdrawal or loss of pleasure. There are no FDA-approved treatments for patients with those needs, so it would be a huge breakthrough if positive efficacy results are produced in the late-stage trial, Colling said — Acadia has said topline results are expected this year.
“Nuplazid has already been approved for Parkinson’s disease psychosis, which would help to support an sNDA for schizophrenia, but in that instance, careful pricing deliberations would have to be made by Acadia in order for the drug to be competitive if it enters the schizophrenia market,” Colling said.
Two drugs designed to target negative schizophrenia symptoms recently ran into trouble.
“Minerva recently received a complete response letter from the FDA for MIN-101 (roluperidone), which was disappointing but not unexpected considering the unconvincing data produced so far,” Colling said. Unless the company can produce different results in an additional study, it may not be able to bring the drug over the finish line, she said.
In addition, Sumitomo Pharma’s plans to submit an NDA for the drug that aims to improve both positive and negative symptoms in 2023 were derailed when two trials fell short due to overperforming placebo groups.
“Sumitomo is likely to continue pursuing an NDA … especially if this large placebo response dwindles in other ongoing trials, although regulators may still wish to see another trial in light of these most recent failures,” Colling said.
Improving treatment compliance
Another area of focus in schizophrenia treatment is improving treatment compliance through the use of long-acting injectable (LAI) neuroleptics.
“LAIs are now recommended by the American Psychiatric Association, as well as others, as a first-line treatment for patients with severe and persistent mental illness,” Colling said. “LAIs are being increasingly prescribed by physicians to increase patient adherence since poor medication compliance rates are seen all too commonly.”
Johnson & Johnson’s Invega Sustenna (paliperidone palmitate) became the first LAI treatment in the schizophrenia market with once-monthly dosing in 2009, followed by Invega Trinza, which can be dosed once every three months, and Invega Hafyera, which is the first and only LAI dosed once every six months, Colling said.
“Other LAIs approved for schizophrenia include Otsuka and Lundbeck’s once-monthly Abilify Maintena (approved by the FDA in 2013) and Alkermes’ Aristada (aripiprazole lauroxil), which was first approved by the FDA in 2015 and is dosed once monthly, every six weeks or every two months,” she said.
Another drug is Abilify Asimtufii, with dosing every two months. While these drugs are more expensive than oral antipsychotics initially, they may ultimately save money by increasing compliance and making relapse less likely, she said.
But injections have drawbacks, so Lyndra Therapeutics is currently testing an oral long-acting version of one of the most commonly prescribed antipsychotics, risperidone. The drug would be taken weekly, preserving the advantages of a long-acting formula, sans needles.
“We are currently advancing oral weekly risperidone into its remaining pivotal safety study and anticipate results will be announced in 2025, shortly followed by an NDA submission,” said Dr. Richard Scranton, Lyndra’s president of global product development and the chief medical officer. The goal is to help more people stick with treatments.
“We believe addressing how people take their medicines will improve adherence to their medication regimen. Although LAIs are an important option for some, only about 15% of people living with schizophrenia are administered LAIs,” Scranton said. “Reasons for this include their in-office administration, needle-phobia and not feeling in control of one's treatment. A long-acting oral treatment option would have a lot of the benefits of an LAI in the oral pill form that patients prefer.”
If these drugs make it to the market, 2024 may bring the first substantial shift that this market has seen since the 1950s.