A new report from the CDC details what many in the life sciences industry have suspected for months — the COVID-19 pandemic caused a surge in antimicrobial resistant infections, threatening years of progress combating one of the world’s most serious public health concerns.
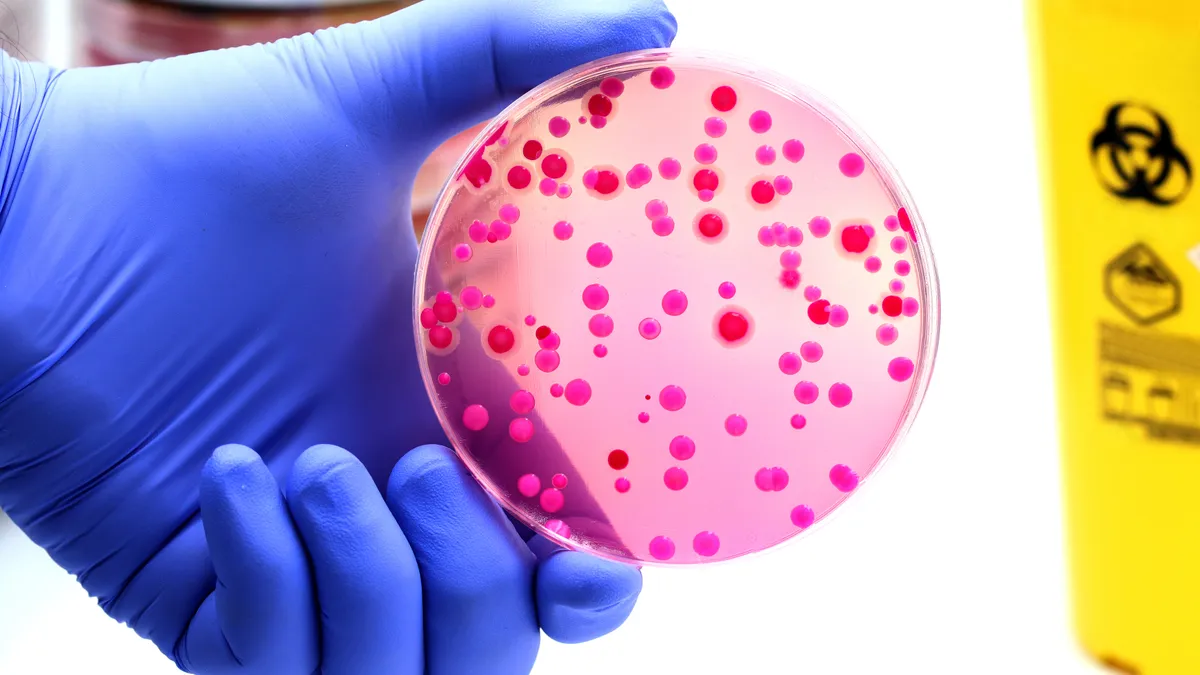
The report, “COVID-19 U.S. Impact on Antimicrobial Resistance,” published July 12, outlines eight bacteria that showed increasingly high levels of resistance to currently available antibiotics during the first years of the pandemic, including pathogens that damage the blood, lungs and skin. Data for nine other major superbug threats, including gonorrhea, forms of Salmonella, strep throat and tuberculosis, are still unavailable due to pandemic-related factors.
Despite the increasing threat, the FDA has not approved any new antibiotics since 2019 when it gave the go-ahead to Nabriva Therapeutics’ drug Xenleta for “community acquired bacterial pneumonia.” And few large pharmas are investing in the area. As of 2021, there were 43 antibiotics in development from 38 companies, only two of which ranked among the top 50 pharmas, according to Pew Research.
The CDC report suggests several ways to increase the U.S.’s superbug fighting capacity, including telehealth services for bacteria contact tracing, specimen self-collection or express clinics, the use of automated data within the National Healthcare Safety Network and partnerships with pharmaceutical companies producing vaccines for certain infections.
“The United States must continue to invest in prevention-focused public health actions, such as accurate laboratory detection, rapid response and containment, effective infection prevention and control and expansion of innovative strategies to combat antimicrobial resistance,” it further recommends.
Here’s a look at where the U.S. stands now: