Members of the House Oversight and Accountability Committee skewered the head of the major pharmacy benefit manager lobby in a hearing on Tuesday over PBMs’ role in rising drug costs, including practices like rebates and spread pricing, as Congress inches closer to enacting legislation to reform the industry.
PBM business practices are a “scam,” said Rep. Stephen Lynch, D-Mass.
“It’s absolutely maddening and I think we have an area here, Mr. Chairman, where we can actually work together and have some bipartisanship,” Lynch said.
The House Oversight and Accountability Committee is one of several government entities currently conducting an investigation into PBMs.
It’s the committee’s second hearing into the middlemen, and the first to include representatives of both PBMs and drugmakers — both of whom attempted to pin the blame for problems in the U.S. drug supply chain on each other.
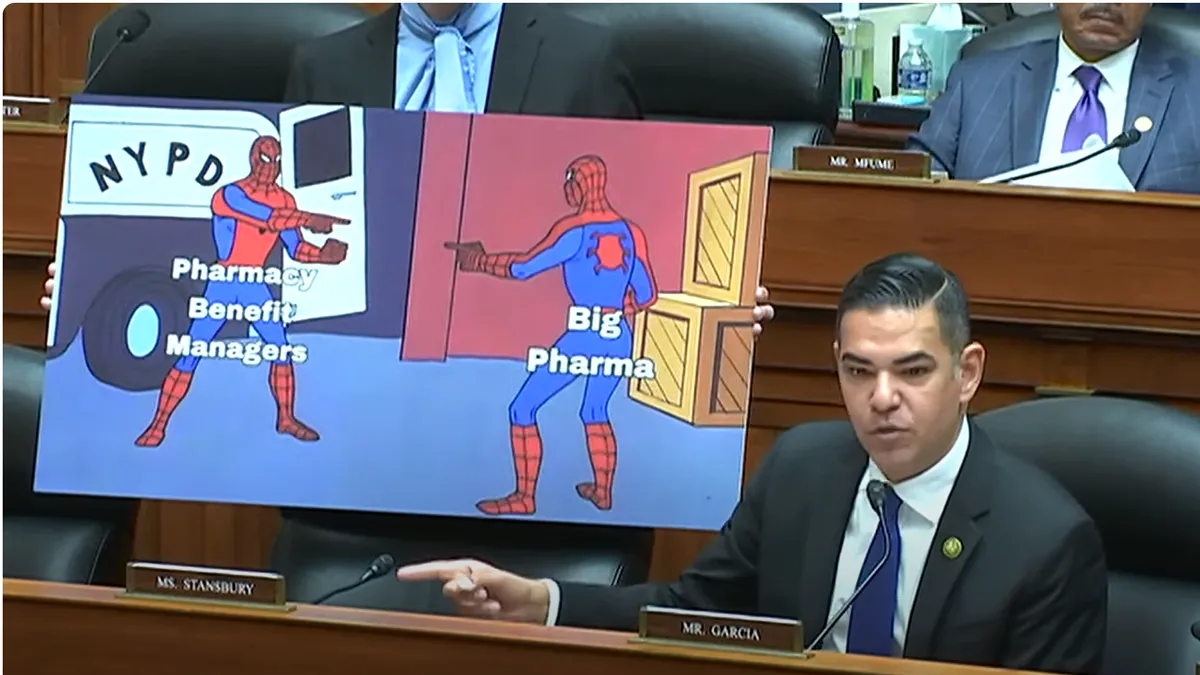
Though PBMs received the brunt of legislators’ criticism during the more than three-hour hearing, pharmaceutical manufacturers did not escape unscathed.
“The big picture here is a lot of fingerpointing,” Rep. Robert Garcia, D-Calif., said. “Both Big Pharma and PBMs are at fault.”
Trading blame
PBMs — the middlemen that negotiate rebates and fees with drugmakers, create formularies and reimburse pharmacies for prescriptions — have been on the defensive amid rising criticism for their role in rising healthcare costs.
On Tuesday, legislators on both sides of the aisle expressed concerns about PBMs’ opaque contracts and controversial business practices.
A major focus of the hearing was rebate arrangements, where drugmakers pay PBMs to have their medications placed on a favorable tier of the formulary. Multiple witnesses testified the rebate structure incentivizes PBMs to prefer drugs with higher list prices, resulting in higher consumer costs.
J.C. Scott, president and CEO of the PBM lobby, the Pharmaceutical Care Management Association, argued that drugmakers continue to hike medication prices regardless of rebates.
PBMs only retain 6% of the drug dollar, while manufacturers retain 65%, Scott said, citing a study backed by the PCMA.
In addition, PBMs pass through most savings to plan sponsors and employers — which are under no obligation to hire a PBM in the first place, Scott said.
“Efforts to lower drug costs must start with an understanding that prices are set by drug companies. When a drug company sets its initial price, that dictates cost throughout the supply chain,” Scott said.
Lori Reilly, chief operating officer of powerful pharmaceutical manufacturer lobby PhRMA, countered that the 6% figure cited by Scott doesn’t take into account the profits PBMs receive from specialty pharmacies.
PBMs limit patients’ ability to access affordable medicines because preferring drugs with higher list prices makes them more money, and PBMs rarely pass negotiated discounts down to patients, Reilly argued. She cited a recent Government Accountability Office report that found Medicare patients paid more than the insurer for 79 of the top 100 drugs.
“While it is true our companies set the list price of the medicine, PBMs are responsible for setting terms of coverage and access and cost sharing that patients have, and their preferences do matter,” Reilly testified.
Craig Burton, executive director of the Biosimilars Council, testified that PBMs frequently restrict access to low-cost generic and biosimilar medications by not including them on formularies because of financial incentives pushing them toward high-price brands.
Even when generics are covered, they can still result in higher costs for consumers, according to a Wall Street Journal article published last week cited by multiple lawmakers in the hearing.
The article found that PBMs overcharge on generic drugs by thousands of dollars when patients fill prescriptions at in-house pharmacies, allowing them to profit from the higher prices.
Consolidation
Multiple lawmakers said they were concerned about rampant consolidation in the PBM industry. Many PBMs now operate retail and specialty pharmacies, and the biggest PBMs are all owned by major health insurers.
Three PBMs — Caremark, owned by CVS; Express Scripts, owned by Cigna; and OptumRx, owned by UnitedHealth Group — control roughly 80% of the market.
That consolidation has created anticompetitive markets that allow PBMs to leverage market power to profit at multiple points of the pharmaceutical supply chain, said Rep. Jamie Raskin, D-Md., the ranking member of the committee.
Rep. Jake LaTurner, R-Kan., asked Scott to explain how one cancer drug cited by WSJ could be purchased for as little as $55 a month, but cost $6,600 a month for a patient covered by Caremark or Express Scripts.
Scott said price differences could be due to a slew of factors.
“There may be multiple versions of the same generic drug with different price points and also different issues about supply availability, which have to be taken into account,” Scott said.
“So you’re saying there is a scenario by which it would be fair and reasonable that it could cost $55 a month for generic, but if you have CVS or Cigna it’s $6,600 a month? There’s a scenario in your mind where that makes sense and that’s fair?” LaTurner said.
Later in the hearing, Scott said a brand drug might beat out a generic on the formulary if the brand drug lowers its price following competition from the generic.
But “that’s not consistent with anything that our research has found,” said Rep. James Comer, R-Ky., chairman of the committee.
“In communicating with all the stakeholders that we’ve communicated with and met with and spent hours with — and we don’t agree on a whole lot in this committee — but we agree that PBMs need to be reformed significantly, especially from a transparency standpoint,” Comer said.
PBMs steering patients to their own pharmacies is also threatening the health of independent pharmacies, testified Hugh Chancy, president of the National Community Pharmacists Association.
PBMs often reimburse independent pharmacies below the cost of acquiring a drug, or hit them with clawbacks like direct and indirect remuneration fees, Chancy said.
“If we don’t have PBM reforms then we’re going to have pharmacy deserts, and not just in rural America,” Chancy testified.
PhRMA’s Reilly also faced questions about drugmakers’ role in rising costs, including skyrocketing list prices and a lack of price transparency in pharmaceutical ads.
“We know that PBMs play a critical role in the pharmaceutical supply chain, but that doesn’t mean that drug manufacturers are being left off the hook,” said Rep. Cori Bush, D-Mo.
Congressional action
Congress is currently considering a number of bills to reform the PBM industry, including healthcare transparency legislation that the House was scheduled to vote on Monday night.
However, the bill was pulled from the schedule over concerns that it didn’t have enough votes to pass.
The bill would require PBMs to give employers detailed data on prescription drug spending, including drug acquisition costs and rebate information.
Increased transparency could help consumers and employers make informed decisions in choosing PBMs and pharmacies. But banning spread pricing and requiring PBMs to pass all rebates to plan sponsors should be approached carefully by lawmakers, because those reforms could have unintended consequences, testified Rena Conti, a health economist and associate professor at Boston University.
PBM reforms would help lower the price of prescription drugs modestly at best and backfire at worst, because PBMs could seek out new revenue streams like upping administrative fees, according to a recent Brookings report.
And past legislation to repeal rebates would add an estimated $180 billion in cost over a decade, because PBMs are currently saving the system money by negotiating with pharmaceutical manufacturers, according to government data.
Still, political will is rising to reform the PBM industry, according to legislator comments on Tuesday.
“We need to have robust debate about this, we need to continue to have dialogue, we need to start exploring options and we need to get something done,” Comer said.