Breakthrough Technology Identifies and Delivers New Pharmacological Treatments for CNS and PNS Diseases
Rhenovia Pharma Technology Improves Neural Network Analysis
In most industries, solutions to complex problems involve computer modeling and simulation (M&S). Rhenovia Pharma uses state-of-the-art M&S to predict the effects of molecules or combinations of molecules on various read-outs of neuronal networks under physiological and pathological conditions. Furthermore, the predicted need for drug combinations requires new and sophisticated delivery methods, able to integrate patient’s unique characteristics. Imagine that it takes the combination of three drugs to optimally treat a disorder. To identify the optimal concentrations of each of these drugs, there is a need to test at the minimum 10 doses for each drug, which translates into 1,000 experiments. To perform these experiments in the laboratory would require several years, while it will take a few days on a computer cluster. It is this gain in both time and money that constitutes Rhenovia’s innovation, strength, and value.
It becomes more and more apparent that the majority of diseases are multifactorial and multigenetic. This is particularly true for diseases of the central and peripheral nervous systems. Even in the case of diseases caused by single gene mutations, such as Huntington’s disease, the resulting consequences are so complex that in most cases, researchers have not yet been able to come up with a treatment, even less with a cure. As gene therapy has not yet matured to the point where it can safely be used, there is a clear need to identify new approaches for drug discovery and development, which could facilitate and speed up the process of finding new therapeutics for these complex diseases.
Rhenovia is a healthcare SME providing innovative solutions to optimize the development of new medications for the treatment of neurological diseases. Rhenovia develops simulators of physiological mechanisms and functions, which are experimentally validated and trained for predictive in silico studies. These simulators are then integrating findings in patients and postmortem tissues (neuropathological changes and mutated gene-related pathways) to generate simulators, which reproduce various pathological states. These are used to determine in silico the impact of pathophysiological molecular defects on functional biochemical and electrophysiological measures, and identify and validate key molecular targets for drug screening, and establish the most appropriate drug(s) profile(s) for lead optimization and profiling.
Rhenovia has been ranked among the major players of a market estimated at $1.2 trillion in 2017. Rhenovia is viewed as a world leader in the application of biosimulation in the search for treatments of diseases of the central nervous system. In addition, Rhenovia is developing a unique drug delivery system capable of delivering up to seven molecules in a time and dose-dependent manner (Rhepatch). The market for such a drug delivery system was evaluated at $120 billion in 2014.
AEMD Drug Platform Disrupts Metabolic Processes of Cancer Cells
Cornerstone Pharmaceutical’s Technology is Revolutionizing Cancer Treatment
In 2015 in the United States alone, there will be an estimated 1,658,370 new cancer cases diagnosed and 589,430 cancer deaths.
Through its proprietary Altered Energy Metabolism Directed (AEMD) drug platform, Cornerstone Pharmaceutical is creating broad spectrum anti-cancer agents that are novel, highly selective compounds for potentially safer, more effective treatment, which represents a significant global market opportunity.
Highly selective means that AEMD compounds have the ability to target and disrupt the altered metabolism and generation of energy critical for cancer cell growth and survival and not normal, healthy cells in the body.
Cornerstone’s agents do this by targeting and blocking a crucial energy producing pathway required for cancer cell growth and proliferation, thereby destroying cancer cells. A second technology, the Emulsiphan lipid nanoemulsion-based drug delivery system, enhances the selective delivery of therapies through a nanoemulsion approach that results in significantly increased drug concentration in tumor cells several times more than in healthy cells.
Ultimately, Emulsiphan increases cancer cell exposure to drugs contained within this proprietary nanaoemulsion, offering the potential for a safer, more effective drug profile.
The technology produces highly selective and effective agents with minimal toxic effects on normal cells and tissues, which means there is the potential to offer patients safer therapies that are able to destroy the cancer with little to no side effects, providing them with a higher quality of life while undergoing treatment.
Despite decades of significant effort, the achievement of substantial improvements in the treatment of cancer to date has been largely elusive. Current chemotherapeutic treatment options are often non-selective, leading to toxicity to normal cells and tissues and can often limit their optimal use. Many cancer cells have been reported to be distinguished from normal, healthy cells and tissues by their adoption of an altered energy producing metabolic profile. This distinguishing feature creates the opportunity for the creation of new anti-cancer agents with the potential to be highly selective for cancer cells.
Cornerstone’s lead AEMD drug candidate — CP-613 — is a first-in-class anticancer compound designed to disrupt the altered energy-production pathways in cancer cells by targeting their altered mitochondrial metabolism.
CPI-613 has been shown in-vitro to be highly selective in inducing the simultaneous inhibition of two key mitochondrial enzymes involved in cancer cell metabolism: pyruvate dehydrogenase (PDH) and alpha ketoglutarate dehydrogenase (KGDH). Disruption of PDH and KGDH function cuts off the tumor’s mitochondrial energy supply, culminating in cell death.
The technology is based on research led by Drs. Paul Bingham and Zuzana Zachar, who have been pursuing a novel anti-cancer approach that exploits the established differences in patterns of energy metabolism between tumor and normal cells.
Smartphone-Enabled Pill Device Advances Patient Adherence
One World Design’s Technology Advances Patient Engagement
The idea behind the patient adherence technology MedQuarters was born when the CEO and chief operating officer of One World Design & Manufacturing Group listened to Steve Jobs speaking at a conference. They remember the day well. According to CEO Fred Pether, it was June 8, 2009, and Steve Jobs was presenting the new 3GS iPhone at the Apple WWDC meeting. Among the multitude of features Mr. Jobs mentioned, the one that stood out was the new operating system that could drive hardware and software. Chief Operating Officer Matt Coe turned to Mr. Pether and said, “This could drive a smart pill organizer."
Subsequently, One World has designed, patented, and manufactured two versions of a class-one medical device called MedQuarters, which uses wireless technology to continually record and report patient adherence. The important key is that adherence is monitored in real time without the need for patient self-reporting.
The MedQuarters Patient Adherence System not only reminds patients to take their medication, but also educates them along the way so they understand why taking their medication is so important to their health.
The system engages patients using medicine alerts, educational resources, status updates, and rewards. Patients are encouraged to be actively involved in their health in an easy, organized way. Additionally, MedQuarters helps caregivers, health aides, family members, HCPs, and pharmacists to monitor and keep track of patient dosing.
This is particularly important as it gives one central and organized system for the patient’s medication. In other words, everyone who needs to be in the loop is in the loop.
With more than 75-plus reminder apps already on the market, One World decided to not reinvent the wheel and partnered with a software developer. The MedQuarters Patient Adherence System is available to health insurance companies, ACOs, and other healthcare organizations whose operations are dramatically impacted by patient noncompliance.
Currently the charge for the device is $10 per patient per month. The second product, MedQuarters for Injectables, is $5 per patient per month.
MedQuarter’s impact can be seen in the improved dialogue that is established between all parties responsible for the patient’s health. This extends to pharmaceutical manufacturers in that it creates a channel through which drug companies can communicate with patients.
Cutting Cost of AIDS Treatment In Half
VCU’s New Manufacturing Process Expands Access and Reduces Cost
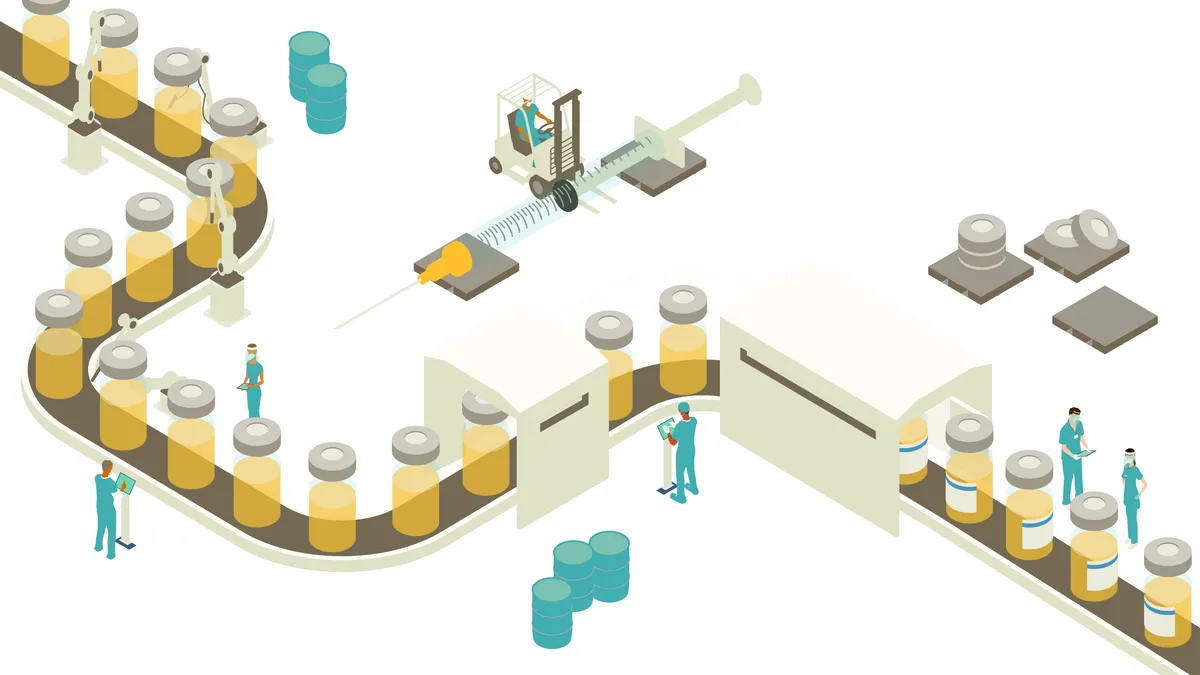
Researchers who are part of a collaborative called Medicine for All have developed a process that will reduce the cost of the manufacturing process for the HIV drug nevirapine by up to 50%. This breakthrough has the potential to greatly expand access to the much-needed drug in countries with emerging economies, such as South Africa.
Led by Frank Gupton, Ph.D., chair, Dept. of Chemical and Life Science Engineering at Virginia Commonwealth University, the group has developed a new pharmaceutical synthesizing technology that will deliver the same quality of drug with the same efficacy as the existing drug at a much lower cost.
The team has holistically applied the principles of modern synthetic chemistry, advanced analytical methodologies, and next-generation processes to complete the first phase of the project, which was to develop a significantly more cost-effective way to produce the starting ingredients of nevirapine.
The project is being conducted in partnership with the Clinton Health Access Initiative and includes researchers from the University of Washington, Florida State University, and the Massachusetts Institute of Technology.
The initiative is funded by a $4.4 million grant from the Bill & Melinda Gates Foundation. The team is in the process of patenting its technology, and will provide open access to anyone working with the Clinton Health Access Initiative or the Gates Foundation.
In parallel, the researchers are working to automate the process. A site for a manufacturing facility is currently being investigated.
While the project will drastically reduce the cost of the AIDs treatment, the bigger opportunity will come from applying the same principles to other drug manufacturing processes to reduce the cost of active ingredients for other drugs that are widely used.
The World Health Organization (WHO) considers nevirapine a first-line therapy for the treatment of AIDS.
Google Earth Meets Human Body
BioDigital Human Provides the First Cloud-Based Immersive 3D Environment for the Exploration of the Human Body
Just a few years ago, being able to view in 3D the smallest details of the human heart and brain from the comfort of your sofa would have been considered unimaginable. Now, thanks to BioDigital Human, you can. The BioDigital Human provides a virtual body within a “freemium" model-base. In July 2014, the BioDigital Human version 3.0 was launched, and is now available to all Internet users in an accessible, intuitive, and user-friendly platform. Aside from being available to a wide consumer base, BioDigital has provided custom solutions to some of the nation’s leading pharmaceutical, biotech, medical device, and publishing companies.
The BioDigital Human helps patients to better understand pharmaceutical and medical device products, simultaneously improving the patient-provider relationship and the patient’s experience of a pharmaceutical or medical device brand. The need on the public level is as crucial as it is on the industry custom level, since despite dynamic technical advances patient health literacy levels are very low.
The BioDigital Human provides a solution with its interactive, virtual tour of the human body. When integrated with the vast amount of online medical data and health records, the platform has the potential to deliver increasingly personalized views of patient health.
The BioDigital Human is used at Memorial Sloan Kettering Cancer Center in New York. The non-profit Smile Train is using the technology as a simulator to train surgeons to repair children’s cleft palates. The use of the BioDigital Human has had a profound impact on the way surgeons learn this complex procedure, with more than 1 million cleft palate operations performed to date.
BioDigital provides a completely customizable solution to the pharmaceutical and medical device industry, allowing industry leaders to leverage cutting-edge technology for detailed product guides, patient engagement tools, and interactive digital marketing material.
The technology can be embedded within a pharmaceutical marketing site, allowing patients and providers to visualize how a product functions within life-like anatomy. Industry leaders are able to create brand-specific custom applications, using the virtual human to map indications, treated conditions, and detailed anatomy that a patient or provider can easily access and navigate.
The technology can also be used as a training tool that can quickly integrate custom content, allowing sales and marketing teams to better communicate the value of a pharmaceutical or device product to customers.
Reaction from the industry has been positive; BioDigital Human has won a 2014 ON for Learning Award from Common Sense Media as well as a Best Digital Health Resource award from Digital Health Awards.
Stopping Meth Abuse While Curing a Cold
Acura’s Impede Technology Renders Cold Meds Useless to Meth Users
Acura Pharmaceuticals has a long history of recognizing that abuse-deterrent medicines need out-of-the-box thinking and that there is no one-size-fits-all solution. From preventing opioid abuse with Oxaydo, to preventing the use of cold medicine for making meth with Nexafed, Acura is looking at preventing multiple areas of drug abuse.
Acura has disrupted the cold and allergy marketplace with its unique Impede technology that makes Nexafed Sinus Pressure + Pain meth-resistant. Acura’s Impede technology platform is an advanced polymer matrix that disrupts the extraction of PSE from tablets for conversion into the illicit drug methamphetamine. It is an effective cold and sinus solution that also addresses a major public health problem.
Acura recently initiated a pilot clinical study of two experimental formulations of Nexafed (pseudoephedrine HCl) extended-release tablets employing Acura’s second-generation methamphetamine resistant technology, Impede 2.0.
Impede 2.0 in the extended-release formulation has demonstrated, in direct conversion tests performed by an independent, international pharmaceutical services company, the ability to reduce meth-yields, on average, by 75% compared with Sudafed tablets.
Based on Aversion technology proven to work to deter crushing and dissolving of opioid products to facilitate abuse, Acura anticipated applicability to PSE products, since dissolving them in solution is the first step toward extraction or conversion into meth. Developing a formulation that maintained full efficacy for patients comparable to the relief they expect while making the product virtually useless for meth cooks was the challenge, and Impede technology accomplished that objective.
The offering is a game changer for the cold, sinus, and allergy medicine category as a whole. The product is shown to work effectively at relieving nasal and sinus congestion and pain, but is virtually useless to a meth cook. In this case, the status quo was not just ineffective, but caused serious harm in the form of people abusing the product to make drugs. When Nexafed Sinus Pressure + Pain came onto the market, it filled a very specific unmet need for consumers, as there was no nonprescription combination product with PSE and acetaminophen available.
Digitalizing Process Streamlines Clinical Trials
CliniOps’ Technology Shakes Up Clinical Trial Data Collection and Management
CliniOps wants to put the squeeze on clinical trials. The company thinks that a complete digitalization process will reduce time and cost as well as improve trial efficiencies. Through its global solutions technology for eSourcing, monitoring, and patient engagement, the company hopes to address the problems of data capture at trial sites lacking Internet access, among other issues faced by the industry.
At present, monitoring alone accounts for about 30% of a clinical trial’s time and cost. Monitors spend 41% of their time in on-site monitoring and 20% of their time travelling to and from the trial sites. This delays the entire drug development process and leads to substantial additional expenditures. It has been estimated that for each day of delay in the drug-to-market time, the sponsor spends an additional $8 million a day.
To address these challenges, CliniOps developed an innovative eSource solution that allows offline data capture at the source using a tablet-based application. Data are then automatically synched with the application at regular intervals, through trusted Internet access. The hand-held design, user-friendly interface, and workflow-based approach works best at busy clinic environments and is essential in settings without Internet access. Data are available in near real time for reporting and analysis, eliminating the need to wait for manual data entry and extensive auditing.
It is the combination of a Web-based application to set up and analyze clinical trials with an off-line tablet based eSource solution and digitized work-flow that differentiates CliniOps from other solutions.
CliniOps was one of the 16 teams selected to participate in the Center of Entrepreneurship in the Idea to IPO program at the University of California San Francisco School of Medicine.
The focus was how to incorporate the principles of lean startup that are widely practiced in the Silicon Valley startup ecosystem.
The company has also established collaboration and partnerships with other relevant companies in the space, with the goal to leverage existing solutions that work toward an optimal design of the end-to-end solution for the end customer.
CliniOps is shaking up the clinical trial industry by redefining clinical trial data collection and management.
mHealth Paradigm Shifts the Collection of Trial Data
Medidata’s Technologies Have the Power to Improve Clinical Studies
As the use of wearable devices and connected biosensors become more prevalent, sponsors are interested in testing their potential in clinical trials to see if they provide better data than traditional clinical data collecting methods. Medidata is responding to this paradigm shift by piloting mHealth studies that incorporate wearable devices to collect extensive, objective patient data in real time — data that identify digital biomarkers and reveal one of the foundational aspects of a clinical study: whether the patient is getting better.
One such pilot was in partnership with GlaxoSmithKline to evaluate the impact of unifying mHealth devices with cloud-based technologies in a clinical trial setting. The focus of the initiative was to assess the capabilities of mHealth tools and evaluate how they could be used to enable a new model for conducting clinical trials that align patient needs with faster study execution and reduced costs. The project showed that the technology worked and that mHealth technologies have the power to collect large volumes of objective data that are not only reliable, secure, and analysis-ready, but also provide continuous insight into the well-being of patients in real time — a discovery that can transform the way clinical trials are conducted. The joint initiative also successfully proved that this type of unified technology can be used to enhance patient engagement, as well as accelerate the pace of innovation in drug development.
The pilot gathered more than 18 million data points per participant per day — far beyond the few hundred data points in a typical trial. The trial captured more than 500 megabytes of data per participant per hour, including auditing information required for clinical data.
The collaboration with GSK created a breakthrough moment that initiated a rethinking of how patients participate in clinical trials and how to monitor their health in their daily lives without always going into a clinic. This has prompted Medidata to move into the stages of developing the right tools, technology, and infrastructure and connecting with other innovative tech partners to collaborate on the concept, process, and operations behind these mHealth-powered initiatives.
The key differentiator in the joint collaboration with GSK was the infrastructure of the technology, which allowed for a more seamless integration process of collecting, downloading, mapping, routing, and analyzing large volumes of data. Medidata’s data science team continues to work closely with GSK to leverage the data from the project and turn it into meaningful insight that can be used to conduct faster and more patient-centric clinical research.
The infrastructure being deployed indicates that mobile devices can support the long-term goal of lessening the burden on patients participating in studies by streamlining routine procedures, eliminating unnecessary ones, and reducing visits to clinical trial sites.
Objective data can enable investigators to have a more holistic, longitudinal view of a patient’s quality of life, allowing them to take a closer look at a patient’s progress day-to-day as opposed to random snapshots in time.
Devices and monitoring technology that can connect with participants’ existing mobile phones will significantly further these efforts by allowing patients to interact with technology they are already familiar.
In the end, Medidata is building a market by not only providing the technology, but also by making the data generated from these technologies obtainable and assessable.
Integrating Investigator and Site Data
DrugDev’s SiteCloud is a Single Hosted Intelligence Solution
DrugDev’s new technology SiteCloud provides a solution to a faster and better way to find investigator sites for clinical trials. This investigator relationship management and data integration tool hosted in the cloud is purpose-built to support clinical research feasibility and site selection functions that enable sponsors and CROs to make more informed decisions. SiteCloud integrates investigator and site data to create mastered profiles from numerous sources, including a sponsor’s internal experience, the DrugDev Network of more than 80,000 opt-in global investigators actively seeking new trial opportunities, and third-party databases. Using SiteCloud, sponsors and CROs can access a single hosted intelligence solution detailing every investigator and site.
To ensure data integrity, SiteCloud is powered by technology called the DrugDev Number, which assigns a unique universal identifier to every investigator and site in its system to eliminate duplicates and resolve missing, out-of-date, or conflicting data concerns. The DrugDev Number may also be used in other clinical systems, including EDC, payments, CTMS, and third-party site databases to create a complete picture of site and investigator relationships and activity across the entire interaction spectrum.
Importantly, the platform also provides robust Web-based query tools with search capabilities and a customizable display, tailored for feasibility, site identification, qualification, and startup.
A sponsor or CRO’s investigator and site data view is mobile-enabled for easy viewing in the field. SiteCloud also powers the Investigator Databank, a global collaboration featuring investigator and site data sharing between Pfizer, Janssen, Lilly, Merck, and Novartis.
Finding the right sites to conduct clinical trials is a critical step in ensuring the success of a study, and this task can be particularly complex in large global studies. With 11% of investigative sites failing to enroll a single patient at a cost of $30,000 to initiate a site and an additional 37% of sites under enrolling for a protocol, it’s no wonder about $110 billion is spent each year on global R&D, with 60% of that amount devoted to clinical trials.
With SiteCloud, DrugDev is advancing best practice for visualizing multiple sources of investigator, site, and protocol data through one single global technology platform. Innovative companies are taking this integration of big data one step further by shifting their focus away from competition on information, and toward data sharing for the purpose of driving further efficiencies for researchers as well as decreasing burden for investigators.
No More Getting Stuck On Compliance
Enable Injections’ Body-Worn Drug Delivery Device Provides Painless Injection
While focusing on reducing or eliminating the pain of children’s vaccinations for a Chicago hospital, the founders of Enable Injections came to realize that it’s not just children who hate being stuck with a needle. The company broadened its scope and developed the Enable Injector, a discrete body-worn drug delivery device that provides a comfortable injection experience allowing patients to continue normal daily activities during treatment. This new bolus injector may improve the self-administration of the more than 900 biologic drugs in development today.
From treatments for cancer, immune disorders, or rare and chronic diseases, using the Enable Injector means patients won’t need to go to the hospital or a doctor’s office for their treatment.
In October 2014, Enable Injections and CSL Behring entered into an agreement for the development of Enable’s drug delivery system to improve the comfort, convenience, and treatment compliance for patients with rare and serious diseases.
Under the agreement, Enable is developing, manufacturing, and selling its innovative delivery device, which was specifically designed for subcutaneous dosing, to CSL Behring for use with one of CSL Behring’s products on an exclusive worldwide basis. CSL Behring manufactures therapies for rare bleeding disorders and immune diseases, and will offer the bolus injector as an option for delivery of certain therapy medicines that it manufactures.
Enable Injections’ technology is what sets it apart from several other companies that develop wearable high-volume injectors. The company’s medical device engineers created a product that optimizes patient comfort by incorporating flow and pressure-control technology.
The Enable Injector is engineered to sense tissue pressure and, in a personalized approach, automatically adjusts the flow rate to the individual to maintain a comfortable injection pressure throughout. The product also automatically warms as the injector fills, in about 30 seconds, eliminating the usual and much reviled 30-minute wait time before injecting.
The Oreo-cookie sized device can be worn comfortably and discreetly under clothing. The tool was designed after 20 human factors (HF) were studied and incorporated into the design. Hundreds of different prototype designs were tested during the product development cycle, with a wide range of user demographics and environments.
The studies challenged two strongly and long-held pharmaceutical industry beliefs: one, that a device should be pre-filled instead of user filled, and two, that an injection should be done as quickly as possible. In the HF studies, patients consistently preferred a user-filled device that automatically warms the drug while the injector fills, eliminating the unpopular 30-minute warm-up time that is often necessary with refrigerated pre-filled injectors.
Patients also opted for a longer injection time if the injection was more comfortable. In fact, patients said injection time is irrelevant if the injection is not painful and doesn’t interfere with daily activities.
Drug delivery experts have called it a “truly revolutionary" development. Analysts expect the new high-volume bolus injector market to grow rapidly as it meets the needs of the emerging biologic drugs market, which is expected to grow to $220 billion by 2018.
Pending FDA approval, the Enable Injector is available for investigational use. After FDA approval, in the next five years the Enable Injector will replace infusions at a health facility for those patients who choose that option. Within the next two years, bolus injectors are expected to be available to the public.
Assessing Risk Before it Arises
ICON’s ECAT Modernizes Trial Monitoring Methodology
The pharmaceutical industry has traditionally used on-site monitoring approaches with significant — often 100% — amounts of source data verification to help ensure patient safety and produce quality data. ICON recognized that this reactive approach, limited in its ability to quickly identify issues and prevent them from recurring, needed to be replaced with a risk-based monitoring methodology.
As part of its patient centric monitoring approach, ICON developed a technology-aided process called ECAT (Error Capture and Action Tool). This process ensures that every clinical trial protocol is assessed for risk before problems arise ensuring that trial monitors and managers, at both central and site levels, are aligned in all of their activities with that risk assessment.
ECAT provides, for the first time, a means of not only delivering a monitoring plan that is proportionate to risk, but also a means of integrating all aspects of quality management, from the planning through implementation to post-study analysis phases specific to each study.
Fundamental to this innovation was the development of an error categorization protocol and the coupling of that protocol to an online system that allows site monitors to record errors and to take the correct level of mitigation, as determined by the risk management plan.
Site monitors have a study-specific, risk-managed framework within which to operate in preference to non-targeted, blanket 100% source data verification. The approach not only reduces costs, but also improves quality at levels many risk-based monitoring approaches do not address.
The ECAT technology allows the site monitor to generate an audited trip report with full oversight of both the errors detected and the actions taken to correct and mitigate them. The technology uses a checklist approach that streamlines the monitor’s activities and ensures they are targeted and effective. (PV)
——————————————————-
Technologies
Acura Pharmaceuticals
• nexafed.com/consumer
BioDigital
• biodigital.com
CliniOps
• cliniops.com/products/clinitrial
Cornerstone Pharmaceuticals
• cornerstonepharma.com
DrugDev
• drugdev.com
Enable Injections
• enableinjections.com
ICON
• iconplc.com
Medidata Solutions
• mdsol.com
One World Design & Manufacturing Group/MedQuarters
• patientcompliance.com
Rhenovia Pharma
• rhenovia.com
Virginia Commonwealth University
• egr.vcu.edu