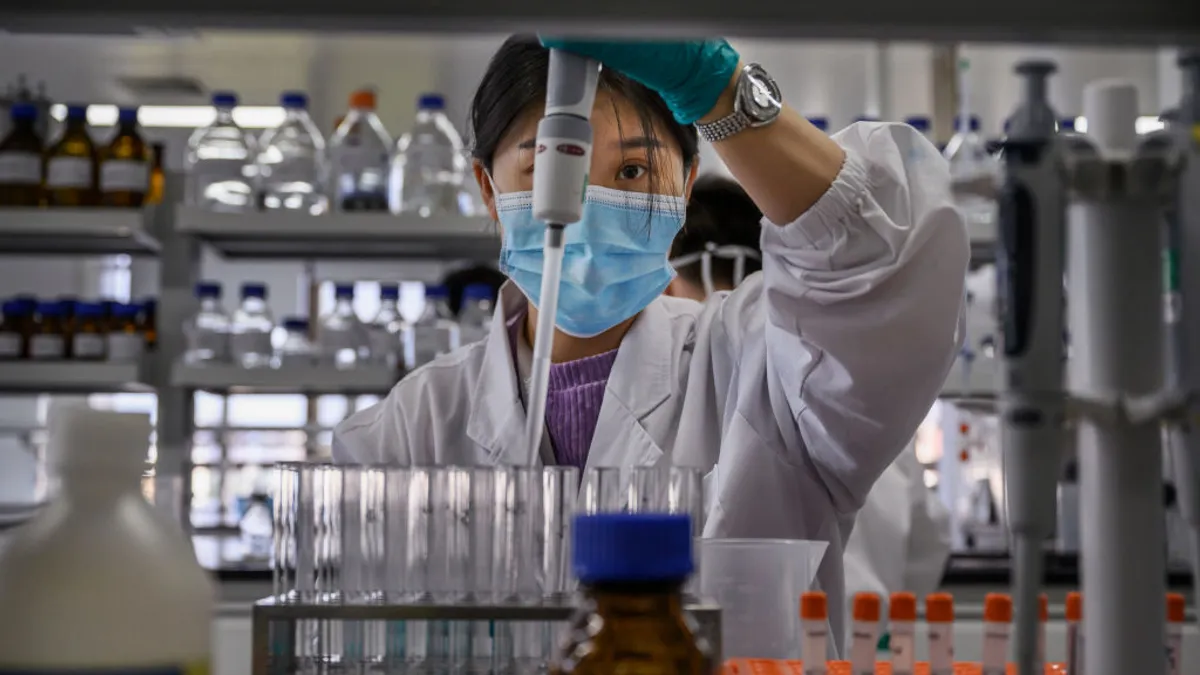
The FDA’s Accelerated Approval Program has helped usher more than 200 drugs to market over the last three decades and in particular, has brought treatments to patients often short on time and options. Since its inception in 1992, the program has become increasingly popular with pharma companies, especially those developing oncology drugs. In fact, the FDA approved more than half of cancer treatments through the accelerated pathway in 2022.
But while the program has been credited for its share of successes, it’s also drawn public ire in recent months. As the pathway used by Biogen to score an approval of its controversial Alzheimer’s drug Aduhelm, scrutiny of accelerated approvals has intensified.
With the pressure on, the FDA is now moving to increase transparency and tighten up this regulatory pathway, ensuring companies carry out confirmatory trials quickly to make certain that approved drugs are safe and effective.
“There are clear advantages when utilizing the accelerated approval pathway, such as providing drugs for unmet needs such as in the rare disease space. (But) this pathway must be utilized in the spirit it was intended,” said Aman Khera, vice president, and global head of regulatory strategy at Worldwide Clinical Trials. “Patients and clinicians … want a drug that is safe and effective. Time will tell how industry reacts and proves itself.”
In the shadow of Aduhelm
The FDA established its accelerated approval program in response to the HIV/AIDS epidemic, which began unraveling in the U.S. in 1981. The goal was to speed patient access to drugs for serious conditions that had unmet needs. To that end, drugs using the pathway aren’t required to show clinical efficacy up front, but instead, demonstrate that the drug improved a surrogate endpoint — such as a marker on a lab test. But for the drug to stay on the market, sponsors must complete confirmatory trials to prove efficacy and monitor for safety.
So far, the accelerated approvals program has lived up to its promise, and most drugs approved using this pathway are still in use today. But some of the program’s flaws were illuminated in the fallout of the Aduhelm failure.

The approval of the high-cost drug, which targets a protein in the brain called beta-amyloid, raised allegations that the process made it too easy for a drug with questionable efficacy to get the green light. The FDA signed off on Aduhelm based on data demonstrating a reduction in the amount of amyloid plaques in the brain and a small improvement in clinical symptoms. However, some thought it should be rejected because the drug failed to meet its primary endpoint in one of its two phase 3 trials, and the ultimate approval raised suspicions that the pathway was used to rescue a drug program without clear evidence that it would truly help patients, said Bridget Silverman, managing editor of U.S. Regulatory Analysis at Citeline’s Pink Sheet.
As criticism of the approval ramped up — three experts from an FDA advisory committee even resigned in protest — the Centers for Medicare and Medicaid Services (CMS) took the unprecedented step of limiting coverage for Aduhelm and other monoclonal antibodies that target amyloid plaques. The agency said it would only reimburse patients participating in clinical trials, and only cover other drugs in this class that receive a traditional FDA approval — a decision that suddenly raised uncertainty about the payer landscape for Alzheimer’s drugs and rattled the industry.
“I think companies are really worried about it,” Silverman said.
Not only are companies leery, but public faith in the FDA has also suffered.
“We are in an era where public trust continues to be of concern in the healthcare space. Development of new drugs is not immune to the underlying current,” Khera said.
Closing a critical approvals gap
Amid the Aduhelm controversy, the Office of Inspector General launched a review of the FDA’s accelerated approval process and its 2022 report found a major gap that the agency has been working to close. Of the 278 drugs approved since 1992, 104 of those had not yet finished confirmatory trials and four approved drugs were five to 12 years past their original completion dates. In addition, 13% of approved drugs were pulled off the market — half of them since January 2021. The lymphoma drug Ukoniq, for example, was in May 2022 after it was linked to a higher risk of death in patients. And it’s not the only drug that ran into safety problems following approval.
"We are in an era where public trust continues to be of concern in the healthcare space. Development of new drugs is not immune to the underlying current."

Aman Khera
VP, global head of regulatory strategy, Worldwide Clinical Trials
One 2017 study published in JAMA found that treatments approved using the accelerated process comprised one of the four groups of treatments that were more likely to have post-approval safety problems. (The other categories were biologics, drugs for psychiatric conditions and “those with near–regulatory deadline approval.”)
To its credit, the FDA has responded to the controversy by taking steps to increase transparency. It’s also tightening up its follow-up process by ensuring that confirmatory studies don’t slip through the cracks and that trials begin quickly — often by the time accelerated approval is granted, Silverman said. The FDA recently also got some regulatory heft to help with that goal through the Food and Drug Omnibus Reform Act of 2022 (FDORA), which was approved at the end of December as part of the Consolidated Appropriations Act, 2023, and gave the agency the authority to require that companies start confirmatory trials before approval or within a specified window if it choose.
“FDA’s May 2014 guidance on expedited programs already said that confirmatory studies ‘would usually’ be underway, so FDORA mostly codifies recent practice while giving some teeth to the agency’s requests,” Silverman said.
In other words, progress is being made.
“A recent example of the new paradigm would be the Biogen and Ionis drug Qalsody (tofersen). At the time of the March 2023 pre-approval advisory committee meeting the confirmatory trial, the study was already half enrolled,” Silverman said.
Another win is that by January 2022, ImmunoGen already enrolled 220 patients in the confirmatory trial for its ovarian cancer drug, Elahere (mirvetuximab soravtansine-gynx), which received accelerated approval in November 2022, she said.
However, this new emphasis on timely confirmatory trials can bring significant challenges for some companies.
“Traditionally, as an industry regulator, I had an early notion that drugs under an accelerated approval would have incentivized the action of conducting the confirmatory study but in the real world, once a drug is out, it has sometimes been hard to have companies undertake these studies, as the product is now in the commercial space of a company,” Khera said.
For some drugs, confirmatory trial delays are due to the challenges involved in testing drugs for rare or fatal diseases that affect a very small number of patients, Silverman said. To overcome these issues, there’s been a push to use real-world data — particularly through registries created by patient-advocacy groups — or claims data. But, Silverman pointed out, because of the FDA’s standards for what constitutes usable data, there are still regulatory kinks with that approach that need to be worked out.
Moving ahead
Despite the recent controversies, the accelerated pathway has brought a number of safe drugs to market including Qalsody (tofersen), the first approved treatment for a rare type of amyotrophic lateral sclerosis (ALS), Daybue (trofinetide) for the rare neurological disorder called Rhett Syndrome, and many more. One 2022 analysis dubbed the accelerated approval program “largely successful” and noted that half of the drugs approved using the pathway go on to gain full approval in a little more than three years. The FDA has stepped in to address those that don’t prove effective, proving the program typically works as intended, Silverman said.
Recent controversies have taken a toll on the accelerated approval pathway’s reputation, but not enough to dampen enthusiasm to continue the program because of the benefits it brings.
“We have seen in the last couple of decades such huge advances in oncology that would have taken much longer before,” Silverman said.
Yet more can be done to ensure that drugs coming through the program are safe and effective for patients.
“One could say the spirit of the accelerated approval process is much the same historically, however we can accept that this pathway is evolving and could (be) regulated with more vigor,” Khera said.