Months of speculation, two leaked drafts and countless disgruntled stakeholder comments later and the European Union’s once-in-a-generation proposal to overhaul its pharma law is finally here.
The long-awaited package published at the end of April aims, through a slew of policy measures, to improve access to medicines across member countries, decrease patient costs and bolster the innovation of new drugs and production of generics. Chief among its broader goals is to decrease the discrepancies between drug launch times across the bloc’s 27 countries and prevent future medicine shortages like those that swept across the continent last winter.
The proposal’s release, however, marks only the beginning of what could be a yearslong process to update the decades-old policies. What comes next is an inevitably long jockeying battle between opposing industry groups and the EU parliament to ultimately reshape the policy.
With such sweeping changes, including a highly criticized shortened exclusivity period for branded drugs, the legislative proposal has caused a motley mix of responses from leading industry players.
Branded manufacturers, from GSK to Novo Nordisk, have been among the proposals’ most ardent objectors, arguing that without more changes, the policy will lead to an exodus of innovation from the bloc as drugmakers struggle to recoup investments.
Meanwhile, Medicines for Europe, a group representing the interests of the generics industry, expressed strong support for the “proposal’s intention to stop the well documented patent gamesmanship and evergreening and the adaptation of incentives to necessary equity of access across the EU.”
The clash between the interests of innovative drug companies and generics groups is just one of many areas where more movement and room for compromise in the EU pharma legislation is likely.

“(The European Commission) wants to get value for money and so on, but they don't want to tip the balance too far such that companies start leaving Europe because that's a real disaster,” Catherine Drew, partner at the international law firm Pinsent Masons, said. “If you compare the size of, for example, the U.S. market versus the European market, there's a disproportionate commercial opportunity there and I certainly don't think that the Commission would want to be disincentivizing investment in Europe.”
Here’s a look at three major areas where pharma could see shifts in policies as the regulation goes through the EU legislative process.
Exclusivity and the Bolar exemption
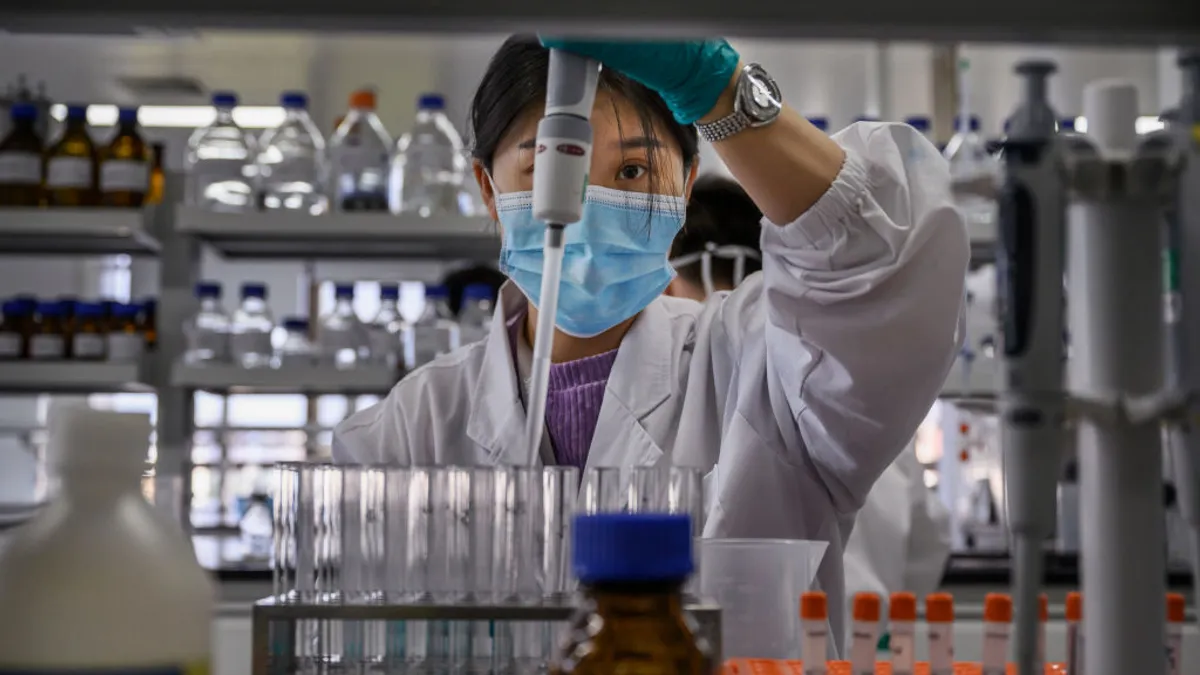
One of the most contentious provisions in the policy package revolves around exclusivity. Currently, branded drugs enjoy 10 years on the market without generic competition, which includes an eight-year period of regulatory data protection. But the new proposal shortens this to just eight years of market exclusivity and adds a slew of incentives that can extend it up to 12 years.
The goal of the policy is twofold: To increase competition and improve access to generics, which have been steadily slipping. A recent report from Medicines for Europe found that, “of all the medicines available 10 years ago, 26% of generic medicines” have disappeared from the European market.
But balancing incentives for the branded and generics market is a tight-rope walk for regulators that could still be swayed, Drew said.
“You don't really want to shift the balance too much in favor of the branded company or too much in favor of the generics. So that's a careful balance that has to be maintained,” she said.
One area where she said there’s potential flexibility is with the Bolar exemption: A provision in the existing EU pharma law that allows studies for regulatory approval of generics and biosimilars to be conducted during the branded drug’s patent period. The Commission’s current proposal aims to broaden the scope of the exemption and simplify the authorization of generics.

Rebecca Guntern, head of Europe at the generic drugmaker Sandoz, said that the current version of the Bolar exemption is “very imprecise and allows for different readings,” but that a “broad and harmonized Bolar exemption is necessary to empower off-patent developers to plan and execute all aspects of the regulatory approval and administrative requirements to deliver on day one competition.”
Specific changes to the scope of the exemption are still subject for discussion, but from the generics perspective, Guntern said an update to the rule should explicitly allow companies to “conduct necessary studies and trials, cover the offer, manufacture, sale, and purchase of patented active pharmaceutical ingredients (APIs) and encompass the subsequent administrative actions.”
Launching medicines across Europe
A key objective of the EU pharma update is to decrease disparities in the time it takes to roll out a drug across the EU — and as such, provisions related to this could shift in the coming months.
Patients in many Central and Eastern European countries, including Slovenia, Poland, Romania and Bulgaria, wait years longer to access medication, on average, compared with Western European countries like Germany and Denmark. For instance, a recent study from IQVIA found the rate of availability, or the number of medicines available to patients, was 66% higher in Germany than in Poland and Estonia.
To fix this, the proposal seeks to provide two years of additional exclusivity to companies that launch their drug across all 27 EU member states within two years. However, industry groups have suggested that this is impractical, and doesn’t fix the main cause of the discrepancy — the patchwork reimbursement system that exists in the bloc.
“The fundamental problem is that paying for medicines is not within the remit of the European Union itself. It's within the remit of each single member state and therefore, to launch a product in 27 member states, you need to go through pricing and reimbursement procedures in each of those 27 member states,” Drew said. “This instrument, therefore might be trying to target something that actually it has no power to deal with.”
Instead, pharma leaders have suggested that the EU pharma policy could be more effective if it requires drugmakers to file paperwork, rather than launch, in all 27 member countries within two years.
Additionally, the European Federation of Pharmaceutical Industries and Associations has argued that the cause of delays in each region varies — in Western Europe it’s a result of value assessment processes, while in Eastern Europe, it’s due to health system constraints, they said in an April report.
"The fundamental problem is that paying for medicines is not within the remit of the European Union itself."

Catherine Drew
Partner, Pinsent Masons
“This shows that there is no one-size-fits-all-solution to fix access issues, and regional or country-specific solutions are needed,” it argued in the report.
Drug shortages
Inflationary pressures, rising energy costs and a suite of other challenges this winter caused worsening drug shortages across the EU. A report by the Pharmaceutical Group of the European Union found that 100% of member countries reported shortages in 2022, with a quarter of countries reporting more than 600 drugs in short supply.
To prevent a similar situation from arising again, the EU Commission outlined a procedure in the pharma update requiring companies to notify the EMA about looming shortages six months before they happen, create shortage prevention plans and hold larger stocks of medicines.
Industry groups, however, have argued that it’s impossible to predict supply chain issues months in advance, and if they could, they’d fix the problem before it arose. A compromise, they say, is creating digital infrastructures that track the consumption of medicines across the EU, which could help them forecast surges in demand.
“The integration of electronic patient information (ePI) along with harmonized forms and presentations for medicines has the potential to revolutionize the way stocks are managed across Europe, effectively avoiding stock-outs and ensuring swift distribution of medications,” Guntern said of the potential policy.
The EU proposal does suggest plans to implement “increased digitalization,” but it remains unclear if policymakers are open to applying digital infrastructures to the drug shortage problem.
And although it is “still in the early stages of negotiations,” Guntern said she is “optimistic that the pharma review will bring positive changes, enabling a more streamlined and digitized approach to healthcare,” when all is said and done.