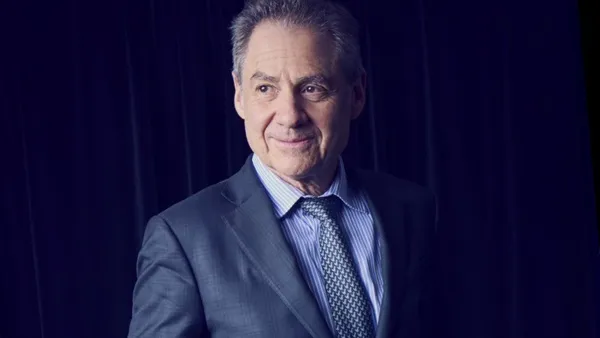
The new legislation surrounding tougher REMS requirements is expected to effect marketing as well as drug development— but the impact might not be all bad. Risk Evaluation and Mitigation Strategies REMS Take Hold BY ROBIN ROBINSON “The key to mitigating risk is applying a rigorous, science-based approach to understanding how physicians and patients actually use medications." Jeffrey Fetterman ParagonRx In the first seven months of 2009, the FDA approved more than 30 Risk Evaluation and Mitigation Strategies (REMS) for both new drug and biologic license applications. There were 24 approvals in 2008, when the REMS legislation took effect. Our experts say it took the industry until the end of 2008 to realize that the new act was going to create a profound sea change in how drugs are developed, approved, and marketed in the United States. The assumption among some in the industry is that if a drug is required by the FDA to have a REMS, there will be a negative impact on market acceptance. Others say this is not necessarily true. But the first step to creating a positive outcome is to be prepared. One out of every three products that earned FDA approval last year required a REMS. Part of that preparation should include thinking about how a REMS program can shape the overall marketing strategy. Depending on the requirements in the medication guides, if a communications plan for physicians is necessary, or if there are access restrictions, marketers will want to determine how to put a positive perspective on risk safety management. “In my experience, many companies do not involve marketing early enough in discussions. They are important participants in the REMS design process because the way the product is commercialized must be consistent with the REMS." Dr. Kelly Davis United BioSource Corp. REMS and Marketing Strategies PharmaVOICE asked industry experts to discuss how a REMS program could and should positively change marketing tactics. Adams. Covance. REMS legislation says the program must be commensurate with the risk of the drug. In the future, the industry and the FDA will have to pay a lot more attention to risk management programs while making sure they are not introducing barriers or even perceived barriers or delays in getting patients their medication. For example, Cimzia, the UCB drug approved for the treatment of Crohn’s disease, was required to submit a REMS, while similar drugs that were approved earlier did not. But three months or so after approving Cimzia, the FDA went back and required the other TNF blockers to also submit a REMS. This may have been an attempt by the FDA to level the playing field or because the agency realized that if one TNF blocker had significant risk to require a REMS, they all did. Regardless, if the FDA had not required the other drugs to provide a REMS, then Cimzia could have been at a disadvantage. For instance, Covance was working on a risk map paradigm for two drugs that had very similar REMS programs, but one drug had fewer requirements in the medication guide. When it came time to market the drug, the company with the fewer requirements used that fact as a marketing tool — almost like counter-detailing. The company told physicians, “If you use our drug, you only have to do steps X, Y, and Z. If you use their drug, you will have to do A, plus X, Y, and Z." Another issue to consider, especially with opioids, is to what extent will access be restricted? There are some who argue that specialty pharmacies for some drugs will reduce access or slow down the receipt of the product. Take the sale of pseudoephedrine, for example, consumers are required to ask for it at the sales counter and show some identification. That is not much of a barrier, but sales of products containing pseudoephedrine have dropped 20% and the less-effective decongestants have taken their place. In this case, one could argue that a relatively modest barrier has had a fairly significant impact on the legitimate use of the product and an increase in sales for the substitution of a less-effective product. These will all be ongoing issues as the REMS requirements become more specific under medication guides. Davis. United BioSource Corp. It is important that the overall commercial strategy, tactics, and messages are consistent with the REMS. Educational materials prepared in support of the REMS should not contain promotional claims, but it is important that they be identified with the brand and are consistent in appearance and content with the commercial materials. In cases where the REMS involves greater control of product distribution, such as a performance-linked access system, marketing tactics will need to focus on ensuring that the appropriate patients do not have significant barriers to product access and that prescribers are well-informed about the potential risks and benefits in order for the product to be used safely. Fetterman. ParagonRx. It is important for companies that are designing a REMS to understand that the FDA is looking for risk communications to be completely separate from promotional communications. It’s clear that the FDA’s concern is that the risk communication will be overwhelmed by promotional communication. In some ways, however, REMS carves out a separate communication program that has to be implemented independently of promotional tactics, which can be a positive thing. While benefit messages are rarely included in a REMS program, there is absolutely nothing that keeps marketers from featuring benefit-risk messages about appropriate use of medications in their non-REMS communications. One advantage of this approach is that it helps the brand meet the REMS’ goals. And if it communicates the appropriate aspects of how to manage those risks, physicians will be more confident, and this could lead to an increase in their intention to prescribe. This could have a profound and positive impact on marketing. A REMS design also can impact physician prescribing. ParagonRx conducted a conjoint analysis among 475 physicians to determine what the affect of a risk management plan such as a REMS could have on their intention to prescribe. The survey showed that if the clinicians judged the program to be burdensome or inappropriately designed, it could have a “profoundly negative impact" on intention to prescribe, and in fact reduced intention to prescribe by as much as 58%. Importantly, a program clinicians perceived as beneficial or appropriate could have a “profoundly positive impact" by increasing intention to prescribe by as much as 42%. Levins. CCC. Companies undertaking a REMS program should not have to change marketing goals, assuming they have been committed to fairly balanced promotion and comprehensive education for their promoted drugs all along. They must, however, change their mindset about REMS to avoid the “black-eye syndrome." A REMS requirement should not be perceived as a brand deficit. The industry must view REMS as a positive versus something that is merely required. By employing educational strategies that reframe a REMS in parallel with its implementation, companies can help stakeholders better understand purpose and value. Ultimately, it’s an opportunity to proactively manage the communication of critical information. According to Wayne Pines, chair of CCC’s advisory board, former FDA associate commissioner, and REMS author, REMS must be viewed by companies “not as a burden, but as an opportunity to position a drug for maximum best use." Provost. INC Research. How an approved product is presented to the medical and consumer communities will depend on the scope and restrictiveness of the REMS. Most REMS that have been approved to date have been medication guides, which do not restrict a product’s distribution or use. These REMS are low impact in terms of product marketing. A REMS that includes “elements to ensure safe use," however, could have a very high impact on product messaging if the elements are restrictive and include a physician and pharmacist certification, or limit where and how the product can be dispensed. Schnoll. PinneyAssociates. Marketing and sales strategies may change based on the nature of the REMS, perhaps influencing rollout strategies or target market priorities. Properly designed REMS should reduce risk and result in a better product on the market. The FDA has been ambivalent as to whether a REMS can be a part of a marketing strategy. Trombetta. Saint Joseph’s University. Companies need to be aware that if the FDA wants to see their marketing plans, it may be able to as a way to clarify how target populations were determined. This can be a land mine; companies are not always careful about what they put into some of their marketing documents. Recent litigation involving overaggressive or inappropriate marketing has revealed how numerous pharmaceutical companies have hoisted themselves on their own petards with careless, off-the-cuff remarks about competitors and internal policies and tactics that would have been better not disclosed. This is a critical issue. When writing an article, people do a spell check; I recommend that marketers start doing a language damage control check — what I call an LDC check — even for internal marketing documents. For example, how were the competitors characterized? Is there language that could be viewed as offensive? I’d recommend removing anything about ROI, and try to phrase everything around a new metric, such as better prescribing practices and how patients are likely to benefit. REMS: Best Practices Our forum experts say companies should start early and anticipate the need for a REMS, no matter how safe the drug. These are just two of the tips that our experts outline as best practices in developing a REMs program. Garg. Amgen. Best practices associated with developing REMS include having a clear understanding of the elements required, obtaining feedback from both internal and external stakeholders, having a dedicated cross-functional team that is empowered to make decisions, and determining roles and responsibilities of each function. It’s also important to develop a project management timeline, outline a governance model, determine the vendor depending on the required elements, and keep the REMS as simple as possible to allow effective implementation. Each REMS is unique based on the requirements of the various elements and the product, and the program is probably not related directly to a therapeutic class. Adams. Covance. The questions asked in the 2005 RiskMAP guidance are worth taking a look at. That guidance looked at the type and magnitude of risk, who was at risk, the existence of treatment alternatives — is it a first-line therapy or last resort — preventability of adverse events per appropriate prescribing, and the most important question of all: would a risk map help with appropriate use? These are the same questions to ask today. Davis. United BioSource Corp. The first decision point is whether a REMS should be proposed for the product in the first place. Of course, every product, whether it’s a drug or biologic, has risks, but not every product will need a formal REMS. For the majority, the information included in the product labeling will be adequate for risk minimization. The main challenge sponsors are struggling with is whether to proactively offer a REMS at the time of submission or to wait until the FDA asks for it. The answer is obvious in some cases, such as a new compound in a class in which predecessor compounds have a REMS, or in situations where the FDA has given clear direction that a REMS will be required. But in most cases it’s a judgment call. Fetterman. ParagonRx. The first priority is to design a REMS that will improve patient safety, and there may be more than one way to do this. The second priority is to create a number of options, then there is an opportunity to define a program that not only improves patient safety but also retains access to medication. If the requirements are burdensome, physicians will avoid using the product and may use a drug that may have an equally challenged risk profile. The third priority is to remember that these programs are only sustainable if they are financially supported by the company, so corporate interests need to be considered in terms of which programs are affordable and sustainable. As long as patient safety and medication access are preserved as priorities No. 1 and No. 2, it is essential for REMS designers to define programs that are fiscally sustainable. Because REMS are relatively new, there is no real, established process in most pharmaceutical companies yet; the majority of sponsors think about developing a risk strategy much too late and end up in crisis planning mode. REMS should be strategized in Phase II and planned during Phase III; it should not wait until clinical studies are completed and regulatory documentation is being developed. In time, the industry will turn to risk management planning sooner. Levins. CCC. Start early, that’s my advice; begin discussing risks in the preclinical phase. Also, think long term; all REMS programs must include a timetable for assessments, with assessments at 18 months, three years, and seven years after approval of the REMS — this is how the FDA checks that the REMS is actually working. Involve communication experts. To date, communications pros have not been squarely integrated into REMS planning teams. This is not productive because REMS are essentially communications programs at the very highest level. Risk information must be understood, resulting in safer use outcomes. Corporate communications, marketing communications, and other messaging veterans should be invited to the strategic planning table when REMS are being designed. Lastly, implementation and follow-up are entirely the manufacturer’s responsibility. Communication with all company employees involved in drug marketing, especially the field salesforce, is vital. Provost. INC Research. Early and continuous risk assessment and mitigation planning will help ensure the most complete understanding of a product’s potential risks and enable a well-conceived REMS to be developed if the need for one arises. Ensure that a multidisciplinary team is engaged in the REMS process — epidemiology, safety, R&D, brand management, regulatory, and legal will all play important roles in a plan’s development. Sponsors need to be proactive in their REMS discussions with the FDA. Avoiding early discussions of how potential safety signals will be addressed can cause unnecessary delays once a product is under formal review. Schnoll. Pinney. REMS differ between and within therapeutic classes based on the results of the benefit-risk assessment of the product. The indication, patient population, seriousness of risks, setting for drug dispensing and administration, and other available treatment options all determine a REMS strategy. A REMS should be devised during the drug’s development to ensure the approval process is streamlined and not hindered. Davis. United BioSource Corp. Once a REMS is decided upon, then its development can begin. It is important to know that the FDA has not yet provided detailed guidelines for REMS, so having knowledge of precedent programs is important. The first step is to decide which risk or risks should be addressed by the minimization strategy. The REMS should focus only on those risks for which the company believes added intervention over and above professional labeling and good pharmacovigilance is needed to minimize and assess that risk. The second step is to develop the goals and objectives of the REMS. These will vary depending on the scope and complexity of the plan and may include educational objectives to make sure that prescribers or patients are aware of particular risks. The third step is to decide on the best overall strategy for risk minimization. It is important to choose a customized strategy that will be sufficient to minimize the risk, while still allowing the best access to the product for appropriate patients and being the least burdensome to the h althcare system. The final step is to design an appropriate evaluation plan for the REMS. This basic approach applies regardless of the therapeutic category. Trombetta. Saint Joseph’s University. Now that the industry has caught on to the newer REMS legislation, there are an army of consultants and a host of seminars all designed to help sponsors design a REMS program. However, I don’t think the challenge is knowing or not knowing how to design a REMS program; the key to a REMS program is that it’s going to be 99% strategy and marketing, and not so much about the FDA or legal. In fact, there may be a need for sponsors to use a strategy called “demarketing," which means companies would downplay or defuse the use of the brand, especially in the case of a REMS requiring the product to be administered to a small, targeted patient population. What a REMS program needs to do is make sure the drug gets to only the people who should be using it and that the communication plan guides the physician to use the drug properly. Of course, this will upset the applecart in sales because how does a company compensate its salesforce for selling less? On the other hand, if a physician has to follow the steps of a REMS, now the sales rep has some value to bring to the table by offering to help him or her comply with the REMS. F PharmaVOICE welcomes comments about this article. E-mail us at [email protected].
An article from


REMS Take Hold
Filed Under:
Commercialization